711 Voluntary plans - 1-888-772-9682 TTY. Depends on contract renewal.
Contact us by phone.
Freedom health provider phone number. For inquiries for Medicare Advantage Freedom Blue PPO administered by Highmark Senior Solutions Company please call. The Provider Service Center helps with contracting patient services precertification and many other questions. Freedom Health Inc.
You will need your Member ID number from your ID card and Medicare last four characters from your Medicare card. Enrollment in Freedom Health Inc. Medical Resource Management 5173648560.
Providers Request Access Here. Most popular medical specialty of providers who accept Freedom Health. Is an HMO with a Medicare contract and a contract with the state of Florida Medicaid program.
CHURCH AVENUE Tampa Florida 33614 United States. 711 for more information. Freedom Dental covers a 32 county service area including the Greater Kansas City Metropolitan Area.
Commedicare or call our Customer Service Department at 1-800-550-8722 Monday through Sunday 800 am. With hundreds of general and specialist dentists participating in the network finding a dental provider near you is easy. Most popular medical specialty of providers who acceptFreedom Health in Florida.
To access Freedom Blue PPOs online provider directory you can visit www. FREEDOM BLUE PPO. 258 S Sam Houston Blvd.
Tufts Health Freedom Plan offers a wide range of electronic solutions including member eligibility status benefit information claim submission claims adjustment functionality and. Freedom Financial Centers Corporate Headquarters. Before contacting Tufts Health Plan providers are reminded to refer to the Contact Us page available on the Tufts Health Plan and Tufts Health Freedom Plan public websites to identify the appropriate provider call center.
711 Indemnity and PPO-based plans - 1-888-MD AETNA 1-888-632-3862 TTY. For more recent information or other questions please contact Freedom Healths Member Services at 1-800-401-2740 or for TTYTDD users 711. 866PHPCOMP 7472667 Disease Management Programs Asthma Diabetes Tobacco Cessation 5173648466.
This Information is not a complete description of benefits. Appeals Grievances PO. If you havent already registered for Braven Health.
Up-to-date information about Freedom Blue PPOs network providers in your area you can visit wwwhighmarkblueshield. TTY users should call 711. From October 1 to March 31 we are open 7 days a week from 8 am.
236 years Average ProfilePoints score for Providers who take Freedom Health. New User Sign Up. Call or visit the nearest Freedom Insurance Company location.
HMO and Medicare Advantage - 1-800-624-0756 TTY. Please create a username and password. Location Map Driving Directions.
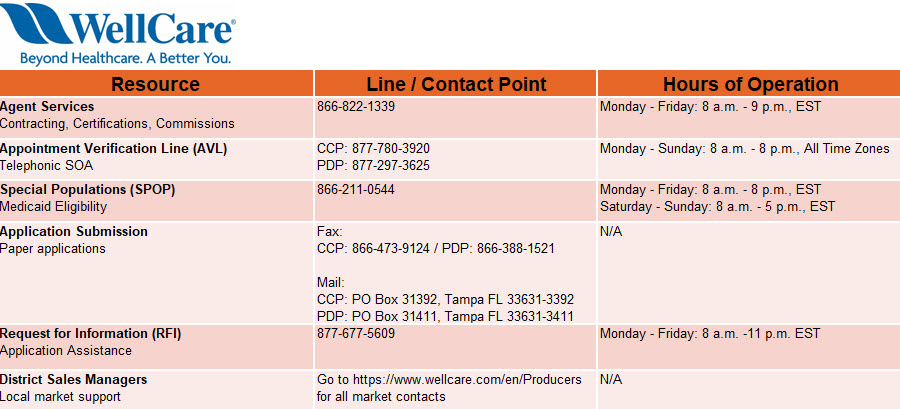
San Benito TX 78586. Braven Health has a separate Payer ID 84367 Providers must use this separate Payer ID for Braven Health for claims and other electronic transactions with Braven Health. Phone numbers are listed by product and state if applicable so the information is easily identifiable.
BOX 152727 Tampa FL 33684 COMPLAINTS APPEALS GRIEVANCES Behavioral Health Beacon Health Options Formerly known as Psychcare 888 273-3710 Chiropractic Chiro Alliance 716 712-2830 Dental Argus Dental 855 445-9757 Diabetic Supplies - OTC Freedom Member Services 800 401-2740. Braven Health dedicated provider phone numbers. Fraud and Abuse Report.
Our hours of operation are.