The Medicaid eligibility limit was 27 of the federal poverty line in Texas whereas this limit was 150 for New York. This was seen for patients with stages 1 and 2 cancers and in those with stages 3.
 Young Cancer Patients On Medicaid At Higher Risk Of Death Say St Louis Researchers St Louis Public Radio
Young Cancer Patients On Medicaid At Higher Risk Of Death Say St Louis Researchers St Louis Public Radio
Part B of original Medicare covers outpatient services such as doctors visits physical and occupational therapy preventive screenings and some medical equipment and supplies.
Medicaid for cancer patients. Also you could enjoy two critical advantages. With this study researchers aimed to assess the associations between state Medicaid income eligibility limits and long-term survival in patients with newly diagnosed cancer. Medicare covers cancer treatment prescribed by a doctor who accepts Medicare.
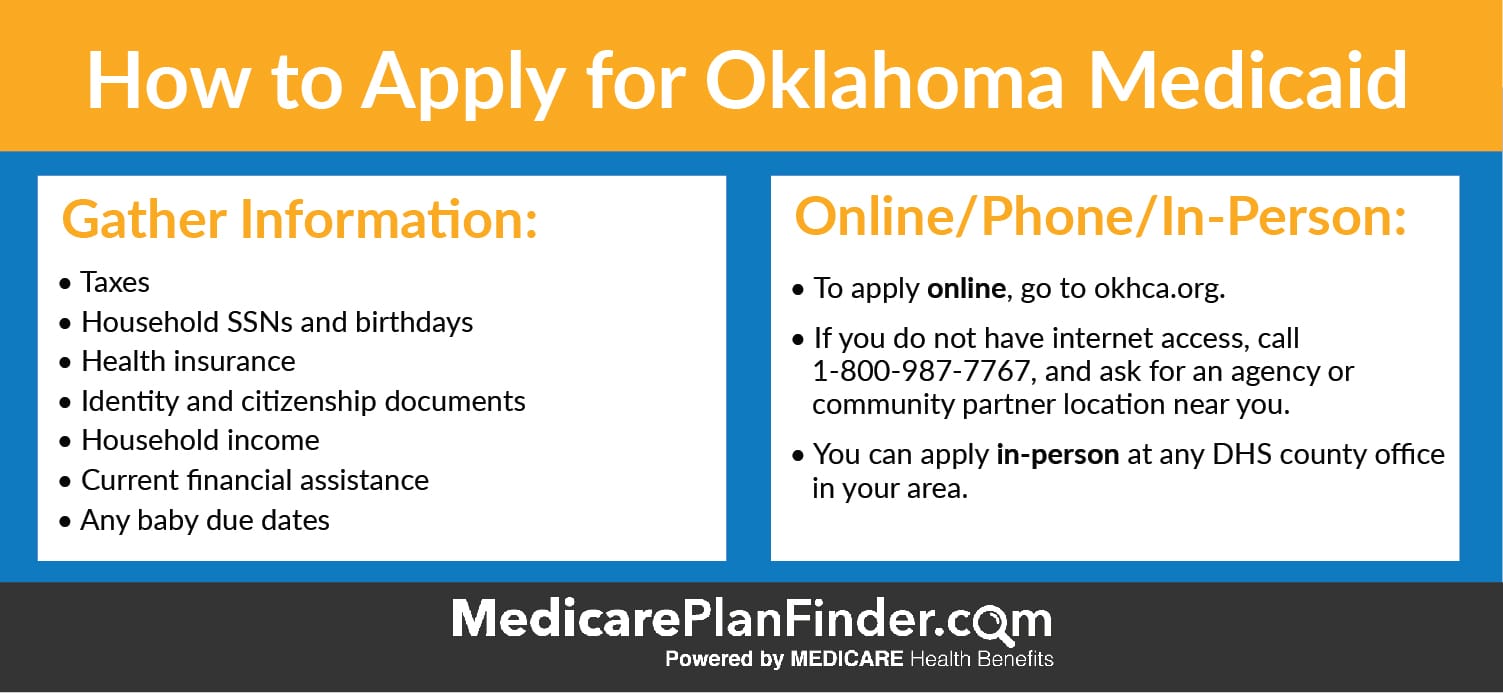
From basic information about cancer and its causes to in-depth information on specific cancer types including risk factors early detection diagnosis and treatment options youll find it here. If you have cancer and are hospitalized Medicare Part A Hospital Insurance will cover a portion of your medically-necessary cancer-related services and treatments according to Medicare Coverage of Cancer Treatment Services a guide created by the Centers for Medicare Medicaid Service CMS. You might be eligible for free coverage depending on your household income and the state where you live.
Medicare pays 80 percent of what your care provider bills. For cancer patients and other individuals diagnosed with a serious medical condition for which expensive treatment is necessary Medicaid provides individuals and families with financial protection. Medicaid is the first place to turn for cancer patients without insurance.
Part D covers outpatient prescription drugs. Whether you or someone you love has cancer knowing what to expect can help you cope. Who pays for home care for cancer patients.
The Breast Cancer Index test has been formally studied in several clinical trials and is recognized by the National Comprehensive Cancer Network NCCN and the American Society of Clinical Oncology ASCO for predicting extended endocrine therapy benefit in patients with early-stage hormone receptor HR-positive breast cancer. Medicare Part A and Cancer Benefits. Researchers found a link between long-term survival of patients newly diagnosed with canceracross all stages and types of the diseaseand expanded Medicaid income.
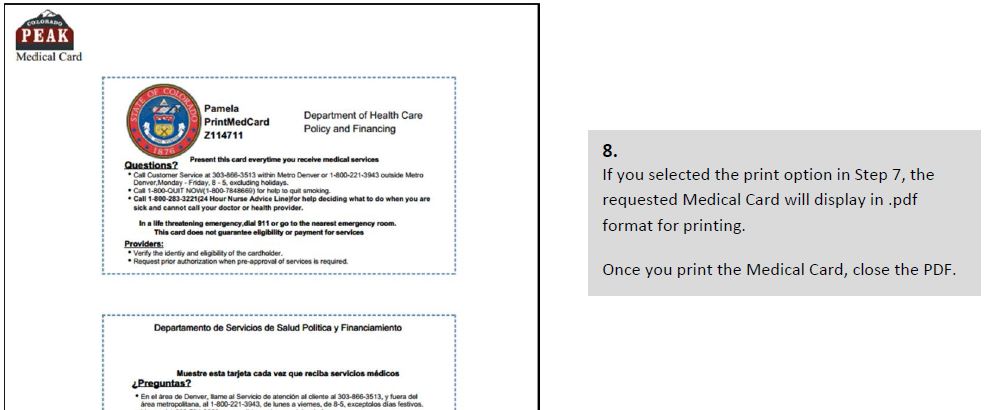
Newly eligible people can begin coverage during the application month with no waiting for open enrollment. Home care services can be paid for by. Medicaid covers the cost of their medical treatment so that they do not have to face financial distress or bankruptcy in order to seek medical care.
These services and treatments include. Berger-Israeloff said that there are charities to help cancer patients too. Patients with cancer who live in states with lower Medicaid income eligibility limits had worse long-term survival outcomes compared with those with higher eligibility limits researchers found.
The researchers distributed patients into four different groups of uninsured patients 60 to 64 years old private insurance patients 60 to 64 years old Medicare patients 60 to 69 years old and. Whether you or someone you love has cancer knowing what to expect can help you cope. Deaths from any cause in states that had income eligibility limits no greater than 50 of the federal poverty level was 31 higher than in 11 states with expanded eligibility.
From basic information about cancer and its causes to in-depth information on specific cancer types including risk factors early detection diagnosis and treatment options youll find it here. Part A of original Medicare covers inpatient hospitalization skilled nursing care hospice and some home care services. Looking at early-stage breast cancer patients who were followed for up to eight years researchers found a strong association between greater Medicaid access and survival.
With Medicaid it can be a disparity between the haves and have-nots When the insurance does not cover all the costs of cancer treatment and people do not have the funds to pay out of pocket Ms. When patients with all cancer types were combined patients who lived in states with the low Medicaid income eligibility limits had the worst survival rates compared with those who lived in states with high limits. Public third-party payers such as Medicare Medicaid and the Veterans Administration VA Private third-party payers such as health insurance companies and managed care plans.