Out-of-network reimbursement is usually higher than in-network allowable. Theyre not in your plans network which means they havent contracted with the insurer on a predetermined rate for their services.
 Out Of Network Out Of Pocket Out Of Options The Unfulfilled Promise Of Parity Nami National Alliance On Mental Illness
Out Of Network Out Of Pocket Out Of Options The Unfulfilled Promise Of Parity Nami National Alliance On Mental Illness
You are in the middle of a complex treatment cycle think chemotherapy or organ transplant when your provider suddenly goes from being in-network to out-of-network.
Out of network provider reimbursement. Depending on the plan you choose and where you live network availability may vary. Sets standards for health plan reimbursement of the out-of-network providers. 1 the in-network providers does not have the appropriate training and experience to meet.
Provide the client with a superbill and have them file the claim to get reimbursed by their insurance company. A referral to an out-of-network provider occurs when. Plans may vary but in general to save on out-of-pocket costs you should visit in-network providers.
If your insurer agrees to let you go out of network at the in-network rate your out-of-network referral will usually be to a specific doctor. It might also happen because your health insurance coverage changed. With out-of-network benefits members may be entitled to payment for covered expenses if they use doctors and other health care professionals outside of the UnitedHealthcare network.
You have two options as an out-of-network provider. The member or health care professional depending on whether or not the member has assigned his or her claim may send a claim for such out-of-network. A members in-network doctor sends a specimen taken in their office to an out-of-network laboratory or pathologist.
This is the option that most out of network clinicians use because this puts most of the work on the client whether this is good or bad is for your decide. Check your out-of-network benefits. But the claims from the other providers may be processed as.
Refer to your plan documents for network details. This might happen because your provider was dropped from or chose to leave the network. One of the lesser known provisions of this legislation requires Health and Human Services the Department to implement rules addressing the amount to be paid to out of network providers who provide emergency services.
Some insurance plans use Medicare fees as a basis for reimbursing service for out-of-network providers. This is the amount of money you have to pay before you are eligible for reimbursement. And establishes the amount that the out-of-network provider would be paid as the greater of 1 the amount the health plan typically pays in-network providers for the same.
When negotiated effectively out-of-network reimbursements can be higher than in-network reimbursements which can increase profitability. 1 murat sarica Getty Images. You will pay the rest.
Referrals for any other health care services are required under a. But typically any doctor managing your care will work with other providers who perform related procedures. Lets say your out-of-network deductible is.
If you see a doctor or other provider that is not covered by your health insurance plan this is called out of network and you will have to pay a larger portion of your medical bill or all of it even if you have health insurance. If your plan includes out-of-network benefits eligible expenses are covered but your out-of-pocket costs may be higher. This is because healthcare providers have the flexibility.
Keep an eye out for these terms. The California law requires state-regulated managed care plans to apply in-network cost sharing to such services. These are typically in the Summary of Benefits included in a member information packet or on your insurance company website.
You can be charged with out-of-network costs when care is provided and the medical provider has not agreed to a negotiated fee with your insurance provider. If you go out of network your insurer may pay for part of the bill. The claim from the original doctor will be processed at the in-network rate.
Absent a law or regulation the non-participating physician can bill the patient for the difference between the amount charged and the insurance carriers out-of-network reimbursement amount. They then multiply that fee by a certain percentage to set the maximum amount that they will pay for that procedure. This means medical providers may charge the full amount for your treatment and your insurance provider may not pay for these charges leaving the full burden of payment up to you.
Out-of-network providers are subject to a different reimbursement structure. Out-of-network care is care you receive from doctors or other providers who dont take your insurance. The rate is often less than what your doctor charges.
A member receives health care services from an out-of-network doctor in an in-network doctors office or practice during the same visit. Insurance Law 4904a-2 and Public Health Law 49041-b require an appeal regarding a referral to an out-of-network provider to be treated as a utilization review appeal and not a grievance if the insured submits a written statement from his or her attending physician that. The Department proposed its interim final rules in the Federal Register on July 28 2010.
 Out Of Network Medical Benefits A Risk Management Primer Employee Benefit News
Out Of Network Medical Benefits A Risk Management Primer Employee Benefit News
 Out Of Network Billing 2 Options For Billing Insurance Simplepractice Blog
Out Of Network Billing 2 Options For Billing Insurance Simplepractice Blog
10 Reasons To Pay Out Of Pocket For Physical Therapy And Dietitian Services Evolve Flagstaff
 Are Out Of Network Benefits Soon To Become Obsolete Mercer Us
Are Out Of Network Benefits Soon To Become Obsolete Mercer Us
Https Swp Mvphealthcare Com Wps Wcm Connect 95456f4c 0de3 4ad7 B441 7cdfb76ce450 Mvp Health Care Outofnetworkcoverage Pdf Mod Ajperes
Https Jassi Org Wp Content Uploads 2013 02 Out Of Network Diy Appeal Packet Pdf
 Saving Money On Therapy With Out Of Network Insurance Benefits
Saving Money On Therapy With Out Of Network Insurance Benefits
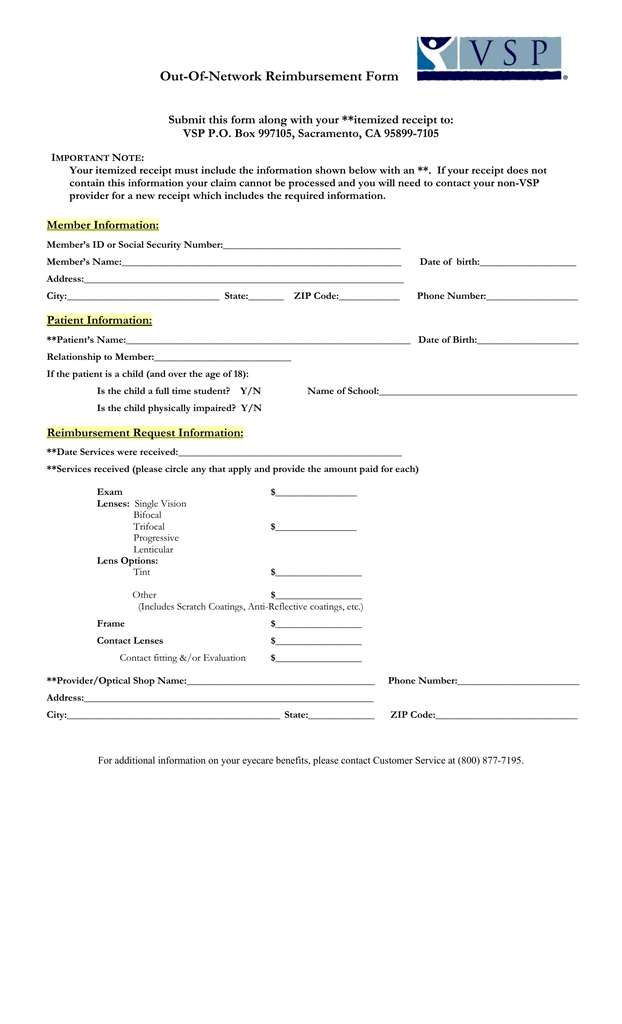 Out Of Network Reimbursement Form
Out Of Network Reimbursement Form
 Reimbursify Launches New App For Out Of Network Reimbursement Claims
Reimbursify Launches New App For Out Of Network Reimbursement Claims
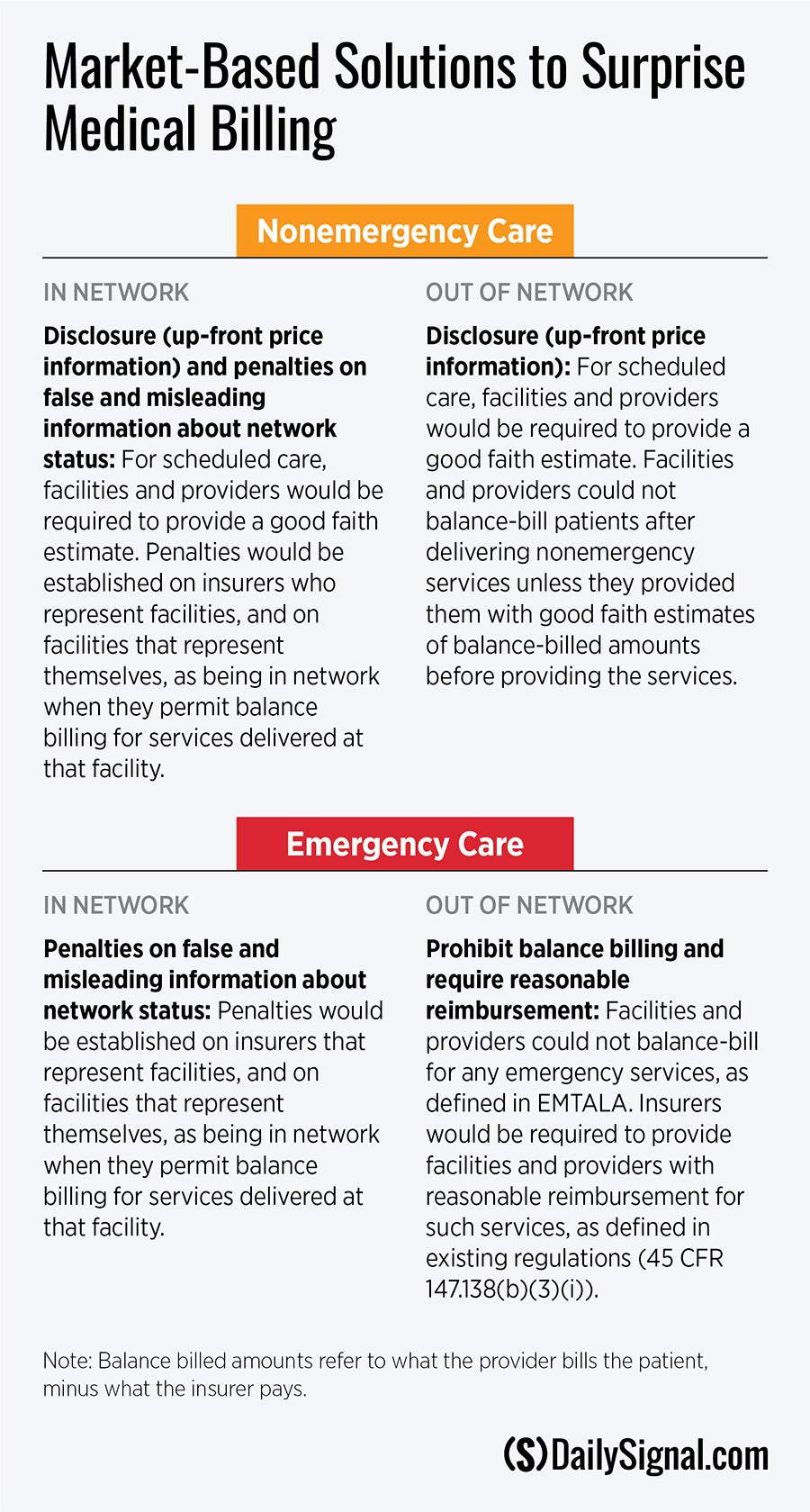
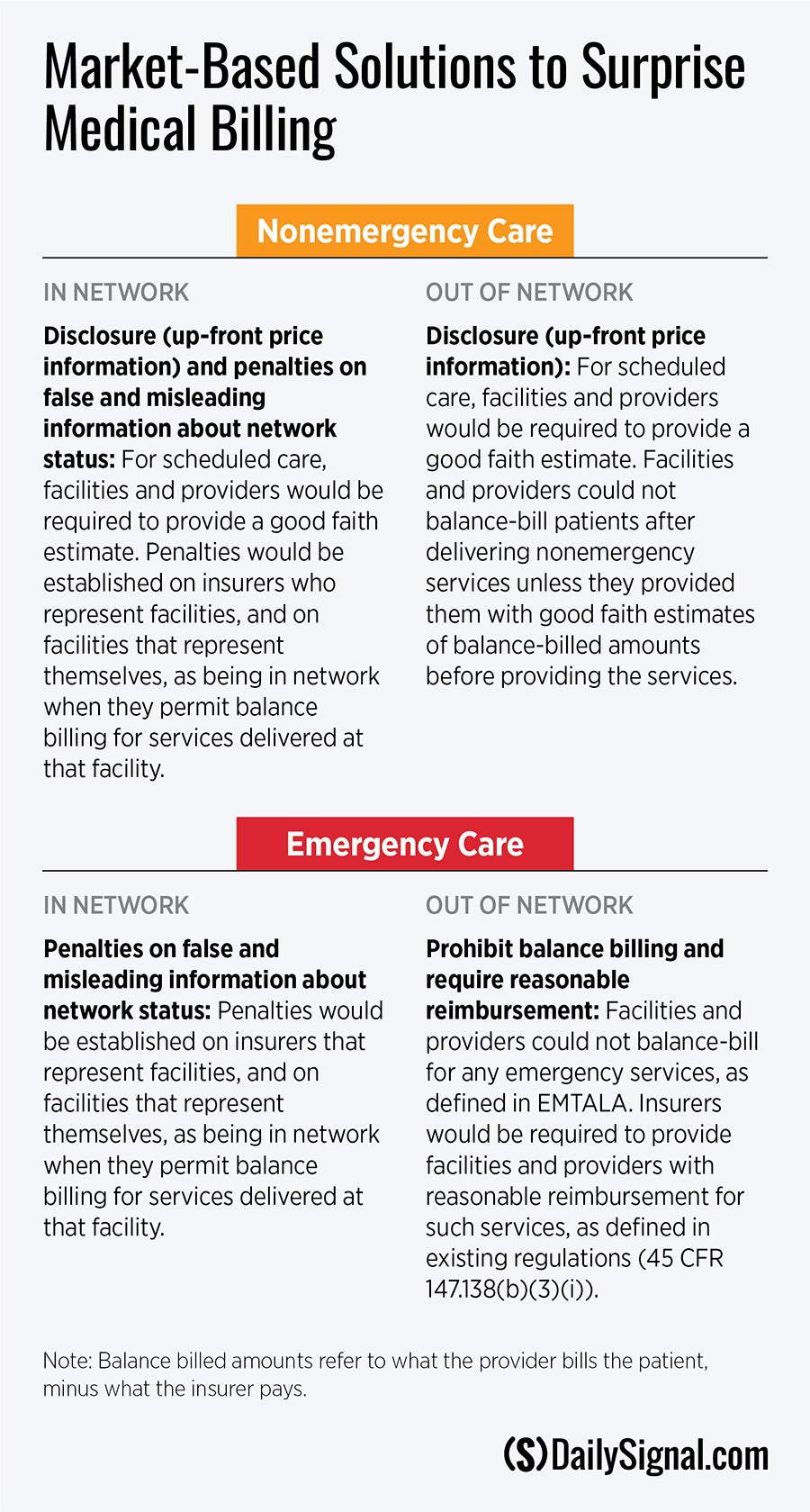 3 Steps To Take The Surprise Out Of Surprise Medical Bills The Heritage Foundation
3 Steps To Take The Surprise Out Of Surprise Medical Bills The Heritage Foundation
Https Www Commonwealthcarealliance Org Getmedia Fb9ba2af 385b 4401 98b7 4cfcfe3c55ba Out Of Network Payment Policy Final
 4 Strategies To Maximize Out Of Network Reimbursement Potential For Lactation Consults Paperless Private Practice For Lactation Consultants
4 Strategies To Maximize Out Of Network Reimbursement Potential For Lactation Consults Paperless Private Practice For Lactation Consultants
 How Out Of Network Reimbursement Works
How Out Of Network Reimbursement Works
Https Www Anthem Com Health Insurance Nsecurepdf English Va Blueviewvision Abcbs Claimform Pdf
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.